HMAA members may access their plan benefits, eligibility, ID cards, and claims information online at HMAA’s portal. Please view the
user guide for instructions.
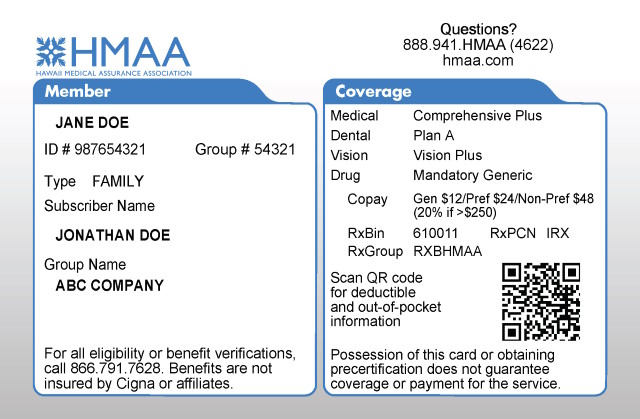
HMAA’s member ID card reflects the cardholder’s plan benefits but does not guarantee coverage or eligibility. It is important for providers to have the most up-to-date information on file and to verify eligibility before rendering services. Therefore we recommend that providers ask patients if any insurance information has changed since their last visit. Providers may also verify eligibility 24/7 via phone at (866) 791-7628 or online.
One ID card is issued to each subscriber (covered employee) and each dependent at least 18 years old or has a different mailing address from the subscriber. Members may contact our Customer Service Center or login to the Online Portal to request additional ID cards or view/print a downloadable version for temporary use.